how to test for diabetes insipidus The renal concentrating mechanism and the clinical consequences of its
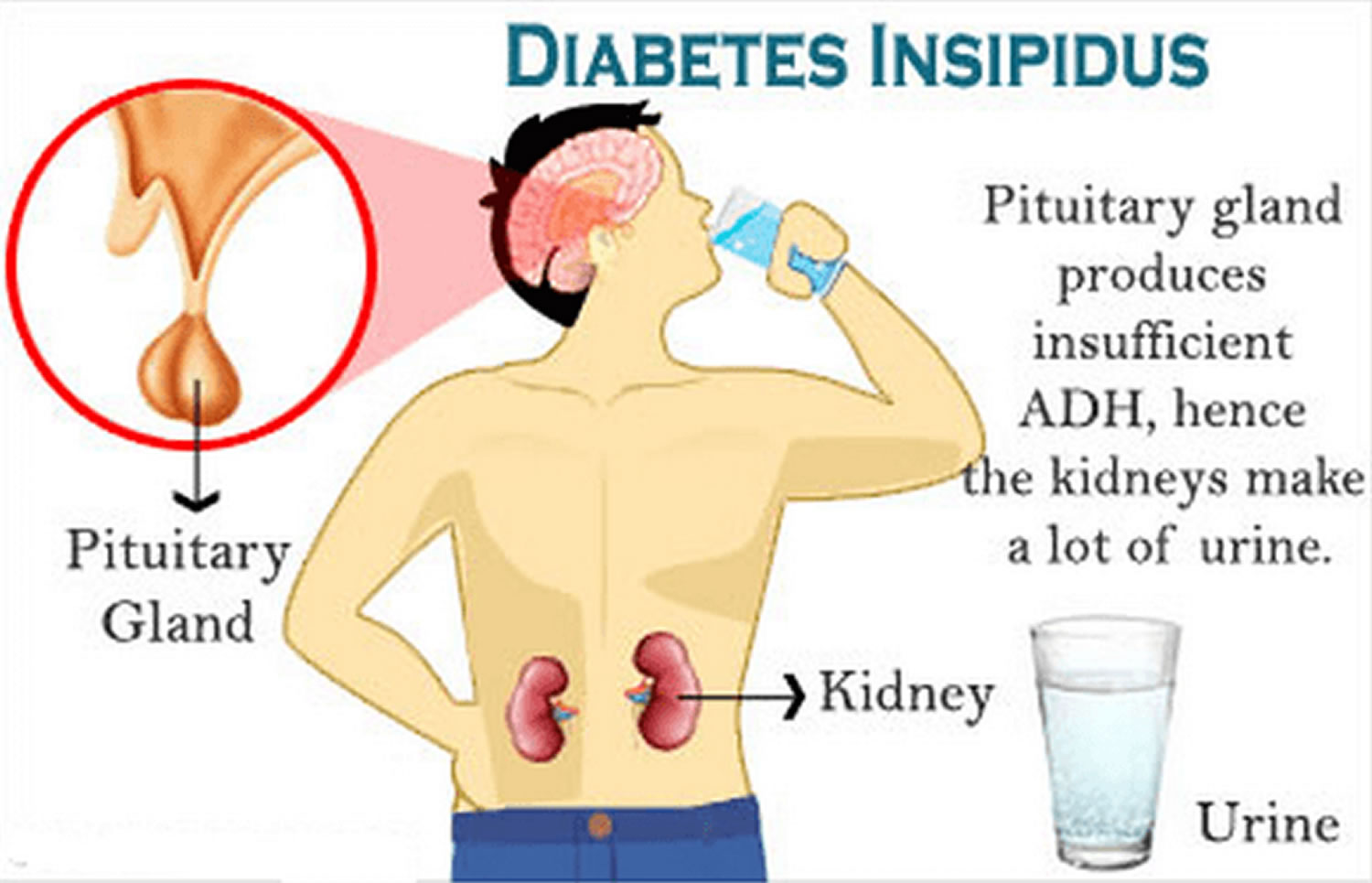
Possible post: Living with Diabetes Insipidus If you have frequent thirst and urination, you may already know that diabetes mellitus is not the only type of diabetes. Another kind of diabetes, called diabetes insipidus, can also affect your body’s ability to regulate fluids. Unlike diabetes mellitus, which involves high blood glucose levels and complications related to insulin, diabetes insipidus involves insufficient antidiuretic hormone (ADH) or kidney response to ADH, resulting in excessive urine production and dehydration. In this post, we will explore the causes, symptoms, diagnosis, and treatment of diabetes insipidus, as well as some tips for managing this condition. Causes: Diabetes insipidus can be caused by various factors that affect the production or function of ADH, a hormone that signals the kidneys to reabsorb water from urine back into the bloodstream. For example, central diabetes insipidus may result from a lack of ADH secretion by the hypothalamus or pituitary gland due to genetic abnormalities, tumors, infections, head injuries, surgeries, or autoimmune disorders. By contrast, nephrogenic diabetes insipidus may occur when the kidneys cannot respond to ADH properly due to inherited mutations, medications, electrolyte imbalances, or chronic diseases such as kidney failure or sickle cell anemia. Gestational diabetes insipidus is a rare form of diabetes insipidus that occurs during pregnancy and resolves after delivery. Symptoms: The main symptoms of diabetes insipidus are polyuria (excessive urine output), polydipsia (excessive thirst), and nocturia (frequent urination at night). Depending on the severity and duration of the condition, diabetes insipidus may also cause dehydration, constipation, dry mouth, fatigue, irritability, confusion, seizures, and even coma. Infants and young children with diabetes insipidus may show poor growth, delayed development, and fever with vomiting. Diagnosis: If you suspect that you have diabetes insipidus, you should see your healthcare provider for a thorough evaluation. The diagnosis of diabetes insipidus usually involves a combination of medical history, physical examination, blood tests, urine tests, and fluid deprivation tests. The fluid deprivation test is a procedure in which you are asked to restrict your fluid intake for several hours while your urine output and body weight are monitored. If you have diabetes insipidus, your urine output will remain high and your urine and blood tests will show low levels of ADH or high levels of electrolytes such as sodium. Imaging tests such as magnetic resonance imaging (MRI) or computed tomography (CT) may also be used to detect any abnormalities in your brain or kidneys. Treatment: The treatment of diabetes insipidus depends on the underlying cause and severity of the condition. In some cases, the symptoms of diabetes insipidus may be managed by addressing the related condition or medication. For example, if you have nephrogenic diabetes insipidus due to lithium therapy, your doctor may switch you to another medication. If you have gestational diabetes insipidus, your doctor may recommend bed rest, fluids, or a medication called desmopressin. If you have central diabetes insipidus, your doctor may prescribe desmopressin, which is a synthetic ADH replacement that can be taken as a pill, nasal spray, or injection. Desmopressin works by reducing urine production and increasing water reabsorption. However, desmopressin should be used with caution, as it can cause water retention, hyponatremia (low sodium), or rebound polyuria if overdosed or abruptly stopped. Therefore, you should follow your doctor’s instructions carefully and monitor your urine output, thirst, and blood electrolytes regularly. Management: Besides medical treatment, there are some self-care measures that you can take to manage your diabetes insipidus and prevent complications. For example, you should drink plenty of fluids, especially water, to avoid dehydration and satisfy your thirst. You should also avoid diuretics, such as caffeine or alcohol, that can increase urine production. You may find it helpful to keep a diary of your fluid intake and output, as well as any symptoms or triggers of your condition. You should also wear a medical alert bracelet or necklace that indicates your diabetes insipidus, in case of emergency. Finally, you should communicate with your healthcare provider, family members, and friends about your condition and needs, and seek support from a diabetes insipidus community or organization. Conclusion: Diabetes insipidus is a rare but serious condition that affects your body’s fluid balance. If you have diabetes insipidus, you may experience excessive thirst, urination, and dehydration, which can impair your daily activities and health. However, with proper diagnosis and treatment, as well as self-care and support, you can live a meaningful and fulfilling life with diabetes insipidus. Remember to stay informed, hydrated, and empowered, and prioritize your health and well-being.
If you are looking for The renal concentrating mechanism and the clinical consequences of its you’ve came to the right page. We have 5 Pics about The renal concentrating mechanism and the clinical consequences of its like Diabetes insipidus | The BMJ, Diabetes Insipidus | Geeky Medics and also #diabetes insipidus tests | Diabetes insipidus, Diabetes test, Diabetes. Here you go:
The Renal Concentrating Mechanism And The Clinical Consequences Of Its
 www.nigeriamedj.comdiabetes insipidus test deprivation water central nephrogenic between table consequences renal
www.nigeriamedj.comdiabetes insipidus test deprivation water central nephrogenic between table consequences renal
Diabetes Insipidus - Causes, Symptoms, Diagnosis & Treatment
 healthjade.netdiabetes insipidus causes symptoms mellitus treatment diagnosis vs google types nursing between contents pituitary kidneys lybrate related posts healthjade
healthjade.netdiabetes insipidus causes symptoms mellitus treatment diagnosis vs google types nursing between contents pituitary kidneys lybrate related posts healthjade
#diabetes Insipidus Tests | Diabetes Insipidus, Diabetes Test, Diabetes
 www.pinterest.cominsipidus healthcheckup
www.pinterest.cominsipidus healthcheckup
Diabetes Insipidus | Geeky Medics
 geekymedics.comdeprivation test fluid di water diabetes insipidus central restriction urine osmolality diagnosis table interpret polydipsia primary results desmopressin partial geekymedics
geekymedics.comdeprivation test fluid di water diabetes insipidus central restriction urine osmolality diagnosis table interpret polydipsia primary results desmopressin partial geekymedics
Diabetes Insipidus | The BMJ
 www.bmj.comdiabetes insipidus polydipsia biochemical fig bmj polyuria assessment
www.bmj.comdiabetes insipidus polydipsia biochemical fig bmj polyuria assessment
Diabetes insipidus test deprivation water central nephrogenic between table consequences renal. Diabetes insipidus. #diabetes insipidus tests